This is not medical advice. Please consult a physician about any of your pregnancy questions and concerns.
One of the most fascinating phenomena, during pregnancy is food cravings. From seemingly mundane cravings for pickles and ice cream to more unusual hankerings for combinations like peanut butter and pickles, pregnancy cravings are as diverse as the women who experience them. In this in-depth exploration, we delve into the science, psychology, and cultural significance of pregnancy food cravings, shedding light on this intriguing aspect of the prenatal experience.
What Causes Pregnancy Cravings?
While the exact cause of pregnancy cravings remains unclear, several factors are believed to contribute to their occurrence:
- Hormonal Changes: During pregnancy, fluctuations in hormone levels, particularly estrogen and progesterone, can influence appetite, taste perception, and cravings. These hormonal changes may heighten sensitivity to certain flavors and aromas, leading to cravings for specific foods.
- Nutritional Needs: Pregnancy is a time of increased nutritional demands, as the body works to support the growth and development of the fetus. Cravings may arise as a subconscious response to the body’s need for specific nutrients such as carbohydrates, protein, fat, vitamins, and minerals.
- Psychological and Emotional Factors: Pregnancy is often accompanied by a range of emotions, including stress, anxiety, and excitement. Food cravings may serve as a coping mechanism or emotional outlet, providing comfort and satisfaction during times of heightened emotional stress.
- Cultural and Environmental Influences: Cultural norms, family traditions, and social influences can shape food preferences and cravings during pregnancy. Expectant mothers may crave foods that are familiar to them or culturally significant, reflecting their upbringing, heritage, and social environment.
While pregnancy food cravings are a common and often harmless aspect of pregnancy, extreme cravings for non-nutritive substances such as clay, chalk, or laundry detergent—known as pica—can indicate underlying nutritional deficiencies or other health concerns. It is essential for expectant mothers to discuss any unusual cravings or dietary changes with their healthcare provider to ensure the health and safety of both mother and baby.
Common Pregnancy Cravings:
Pregnancy cravings can vary widely from woman to woman and may change throughout the course of pregnancy. While some cravings may be for familiar comfort foods, others may be for unusual or unexpected combinations. Some common pregnancy cravings include:
- Sweet Foods: Many pregnant women crave sweet treats such as chocolate, ice cream, or pastries, possibly due to changes in taste perception or a desire for quick energy.
- Salty Snacks: Cravings for salty snacks like chips, pretzels, or pickles are also common during pregnancy, possibly as a result of increased fluid retention or electrolyte imbalances.
- Sour or Tangy Foods: Some women develop cravings for sour or tangy foods like citrus fruits, sour candies, or pickled vegetables, which may provide relief from nausea or stimulate the appetite.
- Spicy Foods: Cravings for spicy foods such as chili, curry, or hot sauce are not uncommon during pregnancy, possibly due to changes in taste perception or a desire for flavorful foods.
- Carbohydrates: Many pregnant women crave carbohydrate-rich foods like bread, pasta, or potatoes, which may provide a quick source of energy and comfort.
- Unusual Combinations: Some pregnancy cravings defy explanation and may involve unusual or unexpected food combinations, such as ice cream with pickles or peanut butter on pickles.
Managing Pregnancy Cravings:
While indulging in pregnancy cravings can provide temporary satisfaction, it’s essential to maintain a balanced and nutritious diet for both maternal and fetal health. Here are some tips for managing pregnancy cravings:
- Moderation: Enjoying small portions of your favorite indulgences can satisfy cravings without overindulging or compromising overall nutritional intake.
- Balance: Aim to balance indulgent cravings with nutrient-dense foods that provide essential vitamins, minerals, and macronutrients for a healthy pregnancy.
- Stay Hydrated: Sometimes, cravings can be mistaken for thirst. Drinking plenty of water throughout the day can help keep cravings in check and maintain hydration.
- Listen to Your Body: Pay attention to your body’s cues and cravings, but also consider whether there may be underlying nutritional needs or emotional factors influencing your cravings.
- Plan Ahead: Keep nutritious snacks on hand to satisfy cravings while still meeting your nutritional needs. Opt for healthier alternatives whenever possible, such as fruit instead of candy or yogurt instead of ice cream.
- Seek Support: Share your cravings and concerns with your healthcare provider, partner, or friends for support and guidance in managing cravings and maintaining a healthy diet during pregnancy.
Conclusion:
Pregnancy cravings are a fascinating and often whimsical aspect of pregnancy that many women experience. While the exact cause of pregnancy cravings remains unclear, hormonal changes, nutrient needs, emotional factors, and cultural influences are believed to play a role. By understanding the underlying factors contributing to cravings and implementing strategies for managing them, expectant mothers can navigate pregnancy cravings with balance, moderation, and nutritional wisdom, ensuring the best possible outcomes for both mother and baby.

This is not medical advice. Please consult a physician about any of your pregnancy questions and concerns.
You are nearing the end of your pregnancy. The phrase I have heard many times by pregnant mothers is, “I am ready to get this baby out of me.” As much as very few mothers look forward to labor, the idea of no longer being pregnant and beginning a new life with a child, makes labor seem like the better option. It is good to be prepared when that time comes. In this article, we’ll explore the signs of labor, what they mean, and when to seek medical attention.
Understanding the Stages of Labor
Before delving into the signs of labor, it is important to understand the stages through which labor progresses. Labor is typically divided into three stages:
- First Stage: Early Labor: During the early stage of labor, the cervix begins to efface (thin out) and dilate (open) in preparation for childbirth. Contractions may start irregularly and increase in frequency and intensity over time. This stage can last several hours or even days as the body prepares for active labor.
- Second Stage: Active Labor: Active labor is characterized by regular and increasingly intense contractions that facilitate the dilation of the cervix to 10 centimeters. This stage typically lasts from a few hours to several hours, culminating in the birth of the baby.
- Third Stage: Delivery of the Placenta: After the baby is born, the third stage of labor involves the delivery of the placenta, the organ that nourished and sustained the baby throughout pregnancy. This stage usually occurs within minutes to an hour after childbirth and is often accompanied by mild contractions and vaginal bleeding.
1. Lightening:
In the weeks leading up to labor, many women experience “lightening,” also known as the baby dropping. This occurs when the baby’s head descends lower into the pelvis, relieving pressure on the diaphragm and easing breathing. Lightening may result in increased pelvic pressure and frequent urination as the baby’s head puts pressure on the bladder.
2. Braxton Hicks Contractions:
Braxton Hicks contractions are irregular, sporadic contractions that occur throughout pregnancy but may become more frequent and intense in the weeks leading up to labor. Unlike true labor contractions, Braxton Hicks contractions are typically mild, do not increase in intensity or frequency over time, and may be relieved by changing positions or resting.
3. Cervical Changes:
As labor approaches, the cervix begins to soften, thin out (efface), and dilate (open) in preparation for childbirth. A healthcare provider may perform a cervical examination to assess cervical changes and determine progress towards labor. However, it’s important to note that cervical changes alone may not always indicate imminent labor and can occur gradually over time.
4. Bloody Show:
A “bloody show” occurs when the mucus plug that seals the cervix during pregnancy is expelled as the cervix begins to dilate. The mucus plug may appear pink, brown, or blood-tinged and is often accompanied by increased vaginal discharge. While a bloody show can be a sign that labor is imminent, it may still be hours or days before active labor begins.
5. Rupture of Membranes (Water Breaking):
The rupture of membranes, commonly referred to as the “water breaking,” occurs when the amniotic sac surrounding the baby ruptures, releasing amniotic fluid. This may happen as a sudden gush or a slow trickle of fluid. If the water breaks, it’s essential to contact a healthcare provider immediately, as it can increase the risk of infection if labor does not progress promptly.
6. Regular Contractions:
True labor contractions are regular, rhythmic contractions that become progressively stronger, longer, and closer together over time. Unlike Braxton Hicks contractions, true labor contractions do not subside with rest or changes in activity and continue to increase in intensity. Timing contractions and monitoring their frequency, duration, and intensity can help determine if labor has begun.
7. Back Pain and Cramping:
Many women experience lower back pain and abdominal cramping as labor approaches. These sensations may feel similar to menstrual cramps and can occur intermittently or persistently as labor progresses. Back pain and cramping are often accompanied by other signs of labor, such as contractions and cervical changes.
8. Nesting Instinct:
Some women experience a surge of energy and an urge to “nest” or prepare for the baby’s arrival as labor approaches. This may involve activities such as cleaning, organizing, and setting up the nursery. While the nesting instinct is not a reliable indicator of impending labor, it can be a sign that the body is preparing for childbirth.
When to Seek Medical Attention:
While experiencing signs of labor can be exciting, it’s essential to know when to seek medical attention. Contact a healthcare provider or go to the hospital if you experience any of the following:
- Regular contractions that occur every five minutes or less
- Rupture of membranes (water breaking)
- Vaginal bleeding or significant changes in vaginal discharge
- Decreased fetal movement
- Severe or persistent abdominal pain
- Signs of preterm labor before 37 weeks gestation
Prepping for the Day:
As labor approaches, it is essential to prepare both physically and emotionally for the birthing process. Here are some tips for preparing for labor and childbirth:
- Attend Childbirth Education Classes: Childbirth education classes can provide valuable information and resources to help you prepare for labor, childbirth, and the postpartum period. Topics may include relaxation techniques, breathing exercises, pain management options, and breastfeeding support.
- Create a Birth Plan: A birth plan is a written document that outlines your preferences and wishes for labor and childbirth. Discuss your birth plan with your healthcare provider and birth team to ensure that your wishes are understood and respected during the birthing process.
- Practice Relaxation Techniques: Relaxation techniques such as deep breathing, visualization, massage, and meditation can help manage pain and discomfort during labor. Practice these techniques regularly leading up to your due date to familiarize yourself with them and incorporate them into your labor experience.
- Stay Active and Healthy: Maintain a healthy lifestyle during pregnancy by eating a balanced diet, staying hydrated, getting regular exercise, and getting plenty of rest. Physical activity such as walking, swimming, and prenatal yoga can help prepare your body for labor and childbirth.
- Pack Your Hospital Bag: Pack a hospital bag with essential items for labor, childbirth, and the postpartum period. Include items such as comfortable clothing, toiletries, snacks, entertainment, and any personal items that will help you feel comfortable and supported during your hospital stay.
- Communicate with Your Birth Team: Open and honest communication with your healthcare provider and birth team is essential throughout the birthing process. Discuss your preferences, concerns, and questions openly, and advocate for yourself and your baby’s needs during labor and childbirth.
- Stay Informed: Educate yourself about the stages of labor, childbirth, and common interventions and procedures used during labor and delivery. Ask questions, seek information from reliable sources, and stay informed about your options and choices throughout the birthing process.
Conclusion:
Recognizing the signs of labor is an important part of preparing for childbirth. While every woman’s labor experience is different, common signs such as lightening, Braxton Hicks contractions, cervical changes, and the rupture of membranes can indicate that labor is near. By familiarizing themselves with these signs and knowing when to seek medical attention, expectant mothers can navigate the final stages of pregnancy with confidence and prepare for the arrival of that bundle of joy.

This is not medical advice. Please consult a physician about any of your pregnancy questions and concerns.
Every week of pregnancy brings new and interesting changes in your body and your child’s development. Just when you thought you had the process down, something changes!
In this article, we’ll outline the key developments and changes that occur during each week of pregnancy, from conception to delivery.
Weeks 1-4: Conception and Implantation
Week 1 marks the beginning of pregnancy, starting from the first day of the woman’s last menstrual period. Despite not being pregnant yet, this week is crucial for calculating the due date. By week 2, ovulation occurs, and conception may take place if the sperm fertilizes the egg. The fertilized egg, known as a zygote, undergoes rapid cell division as it travels down the fallopian tube towards the uterus. By the end of week 4, the zygote implants itself into the uterine lining, initiating the process of embryonic development.
Weeks 5-8: Embryonic Development
By the fifth week of pregnancy, the embryo begins to take shape as distinct layers of cells form the foundation for future organs and tissues. The neural tube, which will eventually develop into the brain and spinal cord, starts to close, and the heart begins to beat, albeit faintly.
As the weeks progress, the embryo undergoes rapid growth and development, with essential organs and structures taking form. By the end of the eighth week, the embryo is referred to as a fetus, and all major organ systems are present, though they are not yet fully developed.
Expectant mothers may experience a range of symptoms during these weeks, including morning sickness, frequent urination, mood swings, and heightened sensitivity to smells. These are the clues that may tell you it’s time for a pregnancy test, if you haven’t already.
Weeks 9-12: Fetal Growth and Maturation
During the ninth to twelfth weeks of pregnancy, the fetus experiences a period of rapid growth and development. Facial features become more defined, and limb movements become more coordinated. External genitalia begin to differentiate, though it may not yet be visible on ultrasound.
Meanwhile, expectant mothers may notice changes in their bodies as pregnancy progresses. The uterus continues to expand, causing the abdomen to protrude slightly. Some women may experience relief from early pregnancy symptoms such as nausea and fatigue, while others may continue to experience these symptoms throughout the first trimester.
Weeks 13-16: Second Trimester Begins
As the second trimester begins, many expectant mothers experience a newfound sense of energy and well-being, often referred to as the “honeymoon phase” of pregnancy. Nausea and fatigue may diminish, and appetite may increase as the body adjusts to the demands of pregnancy.
During these weeks, the fetus undergoes significant growth and development, with facial features becoming more distinct, and bones and muscles strengthening. The fetus may begin to move and kick, though these movements may not yet be felt by the mother.
Expectant mothers may undergo routine prenatal screening tests during the second trimester to assess the health and development of the fetus, including ultrasound scans, blood tests, and genetic screenings.
Weeks 17-20: Maternal Changes and Fetal Growth
By the seventeenth to twentieth weeks of pregnancy, many expectant mothers begin to feel the first flutters of fetal movement, known as “quickening.” These subtle movements may feel like gentle taps or butterflies in the abdomen and are often a source of excitement and reassurance for expectant parents.
Meanwhile, the fetus continues to grow and develop, with the ability to hear and respond to external stimuli such as sound and light. Facial expressions become more expressive, and fingerprints and footprints begin to form.
Expectant mothers may undergo a mid-pregnancy anatomy scan around the twentieth week of pregnancy to assess the fetal anatomy and identify any potential abnormalities or concerns.
Weeks 21-24: Viability Milestone
As the second trimester progresses, the fetus approaches the stage of viability, meaning that it has a chance of survival outside the womb with medical intervention. While the chances of survival increase with each passing week, the fetus is still considered premature and may require intensive medical care if born prematurely.
During these weeks, expectant mothers may notice changes in their bodies as the uterus continues to expand to accommodate the growing fetus. Some women may experience discomfort or pain in the abdomen, pelvis, or back as the ligaments and muscles stretch to accommodate the growing baby.
Weeks 25-28: Third Trimester Begins
As the third trimester begins, the countdown to childbirth begins in earnest, with expectant parents eagerly preparing for the arrival of their baby. The fetus continues to grow and develop, with rapid brain development and increased activity in the womb.
Meanwhile, expectant mothers may experience a range of physical symptoms as pregnancy progresses, including heartburn, indigestion, leg cramps, and difficulty sleeping. It is essential for expectant mothers to prioritize self-care and rest during the third trimester to support their health and well-being.
During the twenty-ninth to thirty-second weeks of pregnancy, the fetus undergoes significant growth and development, with increasing fat deposition and muscle tone. The fetus may adopt a head-down position in preparation for childbirth, though some babies may remain in a breech or transverse position until later in pregnancy.
Meanwhile, expectant mothers may begin to prepare for childbirth by attending prenatal classes, creating a birth plan, and making arrangements for labor and delivery. It is essential for expectant parents to discuss their preferences and concerns with their healthcare provider and birth team to ensure a positive and empowering birth experience.
Weeks 33-36: Final Preparations
As the due date approaches, expectant parents make final preparations for the arrival of their baby, including setting up the nursery, purchasing baby supplies, and packing a hospital bag. It is essential for expectant mothers to stay vigilant for signs of preterm labor, such as regular contractions, abdominal pain, vaginal bleeding, or fluid leakage, and to seek medical attention if any concerning symptoms arise.
During these final weeks of pregnancy, the fetus continues to grow and develop, with increasing weight gain and maturation of organ systems. The fetus may settle into the pelvis in preparation for childbirth, leading to increased pressure on the bladder and pelvis for the mother.
Weeks 37-40: Full Term and Birth
Weeks 37 to 40 mark full term, and the baby is considered ready for delivery. The mother may experience signs of impending labor, such as Braxton Hicks contractions, the release of the mucus plug, and the onset of nesting instincts. The baby may settle even lower into the pelvis in preparation for birth, a process known as “lightening.” Labor can begin at any time during this period, and the mother should be prepared to go to the hospital or birthing center when contractions become regular and intense.
Conclusion:
By staying informed, taking care of their bodies, and seeking support when needed, expectant parents canexperience pregnancy with confidence, resilience, and joy, embracing the act of bringing new life into the world.

This is not medical advice. Please consult a physician about any of your pregnancy questions and concerns.
Pregnancy is a miraculous journey marked by the awe-inspiring process of fetal development. From a single fertilized egg to a fully formed baby, the stages of fetal growth and maturation are a testament to the complexity and wonder of life.
In this article, we’ll delve into the remarkable journey of fetal development during pregnancy, exploring the key stages, milestones, and transformations that occur along the way.
1. Conception and Early Development:
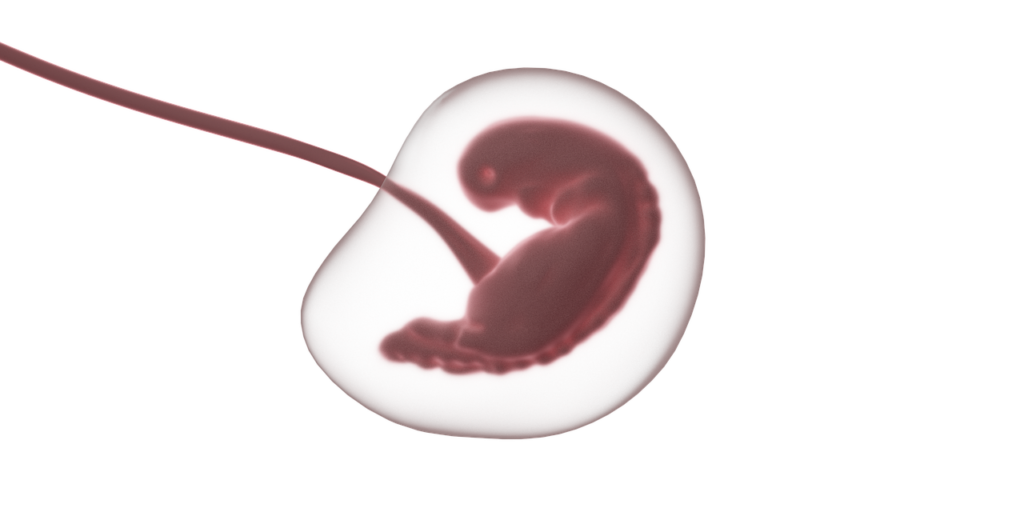
Fetal development begins at the moment of conception, when a sperm fertilizes an egg, forming a single-cell zygote. The zygote then undergoes rapid division and multiplication, forming a cluster of cells called a blastocyst. As the blastocyst travels down the fallopian tube and implants itself into the lining of the uterus, it marks the beginning of embryonic development.
2. Embryonic Development (Weeks 4-10):
During the embryonic stage, which spans from approximately weeks 4 to 10 of pregnancy, the basic structures and organ systems of the developing baby begin to form. Key milestones during this stage include:
- Formation of the Neural Tube: The neural tube, which will later develop into the brain and spinal cord, begins to form early in embryonic development.
- Development of Major Organs: Vital organs such as the heart, lungs, kidneys, and digestive system begin to take shape and develop rudimentary functions.
- Limbs and Facial Features: Limb buds emerge, and facial features such as eyes, ears, and a mouth become visible.
- Placenta Formation: The placenta, an organ that provides oxygen, nutrients, and waste removal for the developing baby, begins to form and take over the role of nutrient exchange from the yolk sac.
3. Fetal Development (Weeks 11-Birth):
After the embryonic stage, the developing baby is referred to as a fetus, and the focus shifts to growth and refinement of existing structures. During the fetal stage, which lasts from approximately week 11 until birth, the fetus undergoes rapid growth and maturation. Key features of fetal development include:
- Growth and Differentiation: The fetus grows rapidly in size and undergoes differentiation of tissues and organs to become more specialized and functional.
- Movement: Around the halfway point of pregnancy, typically between weeks 16 and 20, the fetus begins to exhibit movements, which may be felt by the mother as “quickening.”
- Refinement of Features: Facial features become more defined, and the fetus develops unique fingerprints, toeprints, and other distinguishing characteristics.
- Organ Maturation: Organs and systems continue to mature and develop, with a focus on increasing functionality and readiness for life outside the womb.
4. Third Trimester (Weeks 27-Birth):
During the third trimester of pregnancy, the fetus undergoes significant growth and refinement in preparation for birth. Key developments during this stage include:
- Rapid Growth: The fetus experiences a period of rapid growth, with a focus on gaining weight and increasing in size.
- Brain Development: The fetal brain undergoes significant development, with the formation of intricate neural connections and the maturation of brain structures responsible for essential functions such as cognition, movement, and sensory perception.
- Lung Maturation: The fetal lungs continue to mature, producing surfactant, a substance that helps the lungs expand and function properly after birth.
- Positioning for Birth: In the weeks leading up to birth, the fetus may settle into a head-down position in preparation for delivery, although some babies may remain in a breech or transverse position until later in pregnancy.
5. Conclusion:
The journey of fetal development during pregnancy is a testament to the remarkable capabilities of the human body. From the earliest stages of conception to the moment of birth, each milestone and transformation represents a triumph of nature and a testament to the miracle of life. By understanding the stages of fetal development and the incredible processes at work, we can gain a deeper appreciation for the journey of pregnancy and the precious gift of new life.